
Total Knee Arthroplasty (or TKA) has a longer history than you might think. According to the National Institute of Health, the first knee implants date back as far as the mid 1800s when they “were made from ivory and fixed to the bone using a combination of colophony and plaster of Paris.”
Made from ivory. As in tusks and teeth. 😳
It wasn’t until the 1930s that these parts were replaced with metal and the 1970s that their design was remodeled to replicate the form and function of the actual knee joint. With nearly two centuries of innovation now under its belt, “TKA is the most commonly performed inpatient surgical procedure within the USA and is estimated to reach 3.48 million procedures annually by 2030.” So, count your blessings that you were born in the golden age of knee replacement.
As the largest joint in the human anatomy, the knee is undoubtedly one of the most abused parts of the skeletal system. It bears the weight of the entire upper body and absorbs the shock from every step we take. Over time, its mechanics can degenerate requiring a visit to the doctor, preferably an orthopedic surgeon, who will order x-rays to determine the extent of the deterioration. If the diagnosis is osteoarthritis, the patient may elect to undergo a total knee replacement (also known as TKA) to correct the problem.
What is Total Knee Arthroplasty?
TKA is a surgical procedure where the damaged part of the knee is replaced with an artificial joint made of metal and plastic that is attached to the upper and lower bones of the leg.

How do I know if I’m a candidate for TKA?
Does your knee pain interfere with your daily routine and/or keep you awake at night? Do you struggle to walk short distances? Climb stairs? Sit or stand for extended periods of time? If the answer to any of these questions is yes, you may want to consider this procedure.
I have been scheduled for TKA. What happens next?
Your doctor may recommend a few pre-op sessions with a physical therapist before the surgery. After the surgery, the post-op sessions usually start within a week (sometimes even just a few days) of the procedure. The physician does his or her part to correct the problem. The rehabilitation to regain strength and full range of motion is up you.
At the post-surgical evaluation, your physical therapist will ask about your medical history, chief complaints and long-term goals. Do you want to be able to get around without a cane? Walk the dog in the neighborhood? Keep up with your grandchildren? Travel and sightsee on vacations? Communicate these intentions with your physical therapist and together you can create a plan to get you to your personal finish line.

At the beginning of your treatment, your PT will take measurements of the two main muscle groups – the quadriceps and the hamstrings – that act on the knee. The quadricep muscles are located on the front of the thigh to help straighten the knee while the hamstrings are on the back to help it bend. These numbers determine your starting point for power and flexibility after the surgery. Over the course of your treatment, these measurements will be taken at regular intervals to determine what is and is not improved so your therapist can customize your exercises to keep you on track for your goals.
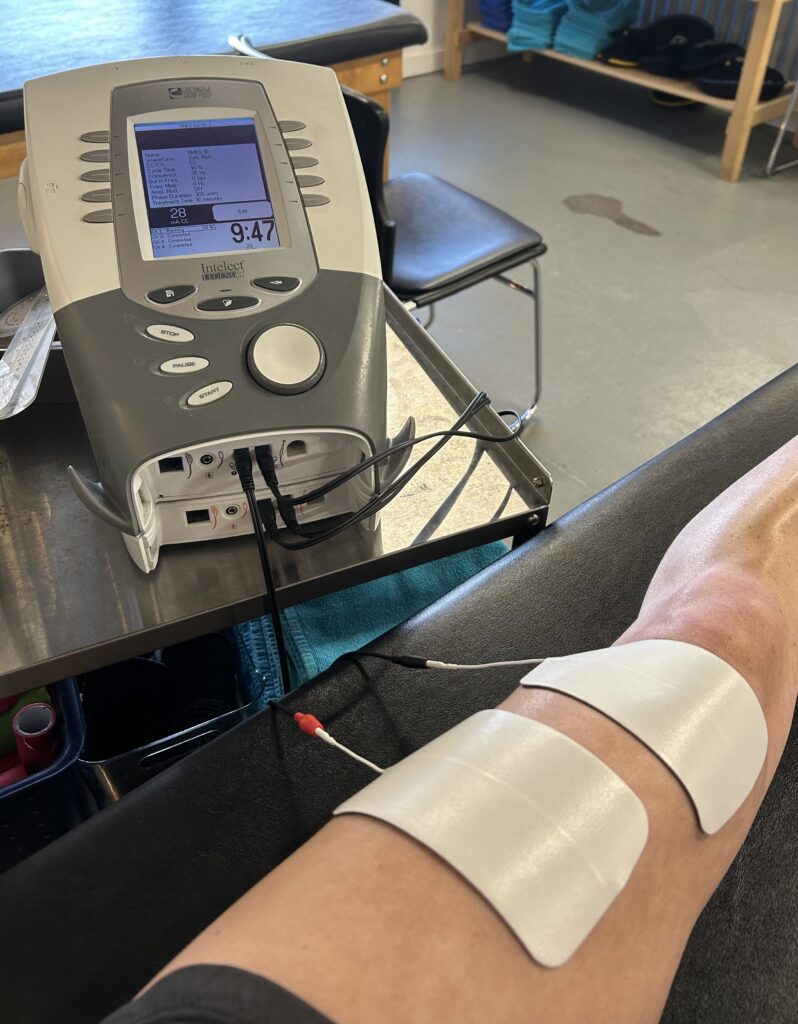
Post-surgical TKA exercises are designed to restore your ability to fully extend and bend your knee as well as bear weight to get you … quite literally … on your feet again. Your treatment plan will start slowly but can eventually include everything from quad squeezes and leg lifts to bike riding and less presses. During and following your in-clinic treatment, you will also receive a personalized home exercise program that you can perform independently to help advance the healing process.
Like we mentioned earlier, the success and rate of your healing schedule are entirely on your shoulders …. or, well, on your knees … as it were.
For more questions about this quality-of-life-changing procedure, please call us (504) 885-8969.
Michele Robert Poche